A team of researchers developed a model showing that irreversible fibrosis development is associated with specific combinations of metabolic and inflammatory cues, building on mathematical modeling work to better understand fibrosis pathogenesis.
Fibrosis is a pathological wound healing in which connective tissue replaces normal tissue to the extent that it goes unchecked, leading to considerable tissue remodeling and the formation of permanent scar tissue. It occurs as the result of constant attempts by injured tissues and infiltrating immune cells to resolve inflammation and repair the damage. In the case of pulmonary fibrosis, the consequences can be devastating.
Substantial challenges remain in our understanding of fibrotic diseases, particularly in the pathogenetic basis upon which they develop. Research suggests that in genetically predisposed individuals, external factors damage the epithelium, initiating an abnormal repair process that causes uncontrolled deposition of extracellular matrix (ECM) material and damage to the tissue architecture.
A team of researchers including Khalifa University’s Dr. Haralampos Hatzikirou, Associate Professor of Mathematics, developed a mathematical model that represents the interplay between processes in the body and reflects the functional effects of inflammation, hypoxia and the adaptive immune context. Their model shows that irreversible fibrosis development is associated with specific combinations of metabolic and inflammatory cues.
Their results were published in Nature Communications.
“Mathematical modeling has proven an invaluable tool in investigating existing biological hypotheses in realistic scenarios or generating experimentally testable ones,” Dr. Hatzikirou said. “We developed a mathematical model of fibrosis based on the in vitro analysis of the interplay between fibroblasts and macrophages in the context of the wound-healing and scarring processes.”
Four core mechanisms are involved in fibrosis, according to the research team. Early inflammatory events involve various immune cells, including macrophages, followed by the activation of fibroblasts, the loss of the regenerative properties of epithelial cells, and the loss of interstitial capillary integrity, compromising oxygen delivery and further promoting the fibrotic process.
Previous models comprehensively describe the central aspects of fibrosis and could predict cell networks leading to clinically observed conditions, but they were limited by the fact that macrophage/fibroblast interactions always occur in the context of specific immunological and metabolic features characterizing the tissue microenvironment. This aspect had yet to be modeled.
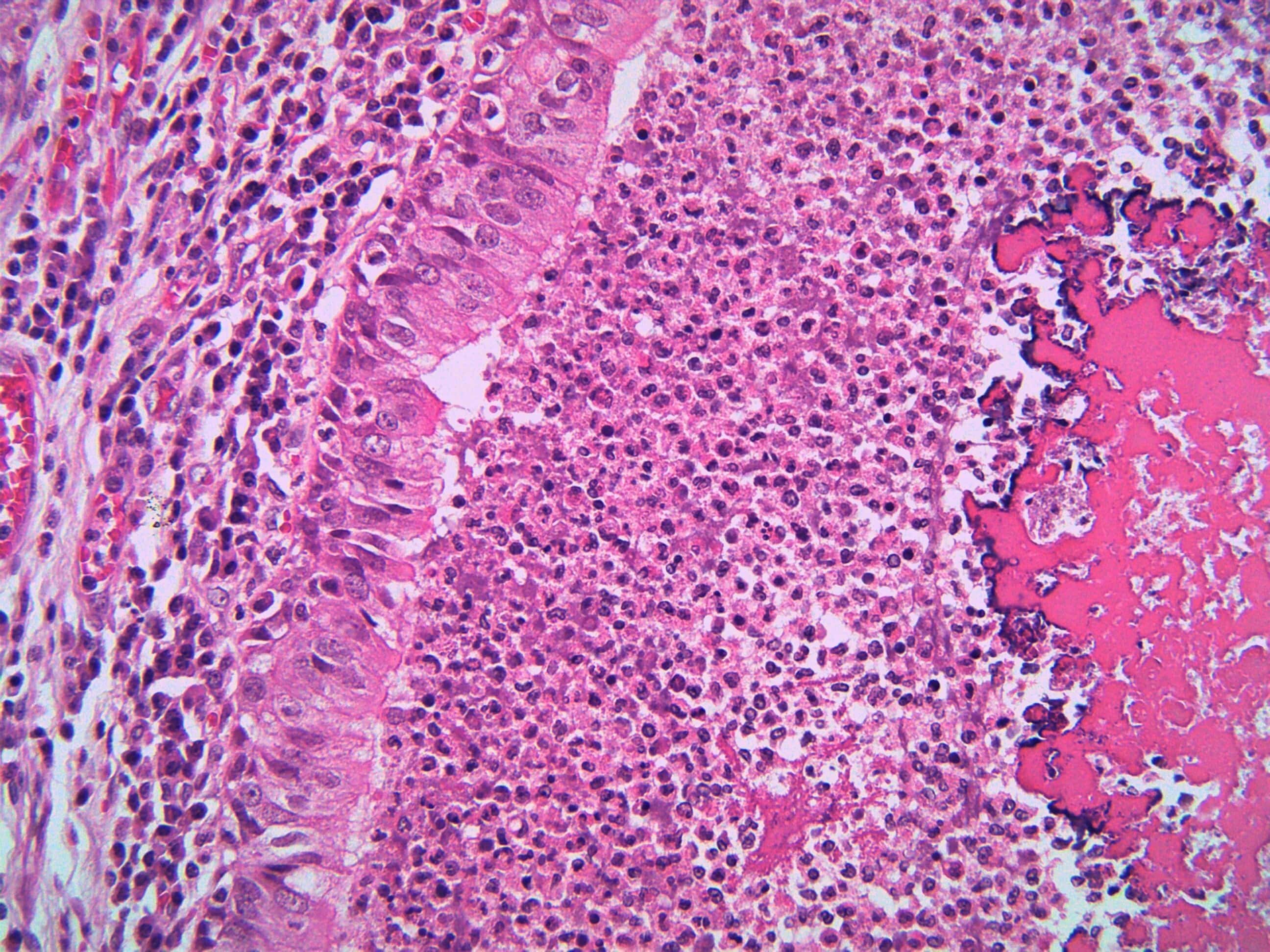
The research team, therefore, developed their model taking this aspect into account. They translated in vitro observations on the relative relevance of different immune and metabolic microenvironmental cues to the macrophage/fibroblast interactions to an in vivo fibrotic scenario. The scenario considered transplanted kidneys, as fibrosis after transplantation is a clinically relevant application case for the model, according to the researchers.
“Our model predicts key interactions for fibrosis development and applies it to tissue sections from human-transplanted kidneys with different degrees of glomerulosclerosis — scarring in the blood vessels of the kidneys,” Dr. Hatzikirou said. “Previous models identified three functional states: a state of healing associated with modest ECM production and two fibrotic states associated with excessive ECM production and either high or low numbers of macrophages, termed ‘hot’ and ‘cold’ fibrosis respectively. Our model allows the implementation of immune and metabolic cues in the current ‘hot’ and ‘cold’ fibrosis model.”
Some of these immune and metabolic cues include hypoxia and inflammation. The researchers noted that effects of inflammation on fibroblasts and macrophages are highly influenced by the tissue environment while the reduction of oxygen induces a metabolic switch in cells causing fibroblasts to assume proinflammatory properties.
“The combination of in vitro and in silico modeling represents a powerful systems medical approach to dissecting fibrosis pathogenesis, applicable to specific pathological conditions, which helps develop coordinated targeted approaches,” Dr. Hatzikirou said. “Our model was validated on tissue-based quantitative immune-phenotyping of biopsies from transplanted kidneys, demonstrating its feasibility. Our model is an innovative approach to analyzing fibrosis pathogenesis and to guiding the development of targeted therapies.”
Jade Sterling
Science Writer
24 January 2023