The Worldwide Burden of Colorectal Cancer and its Risk Factors
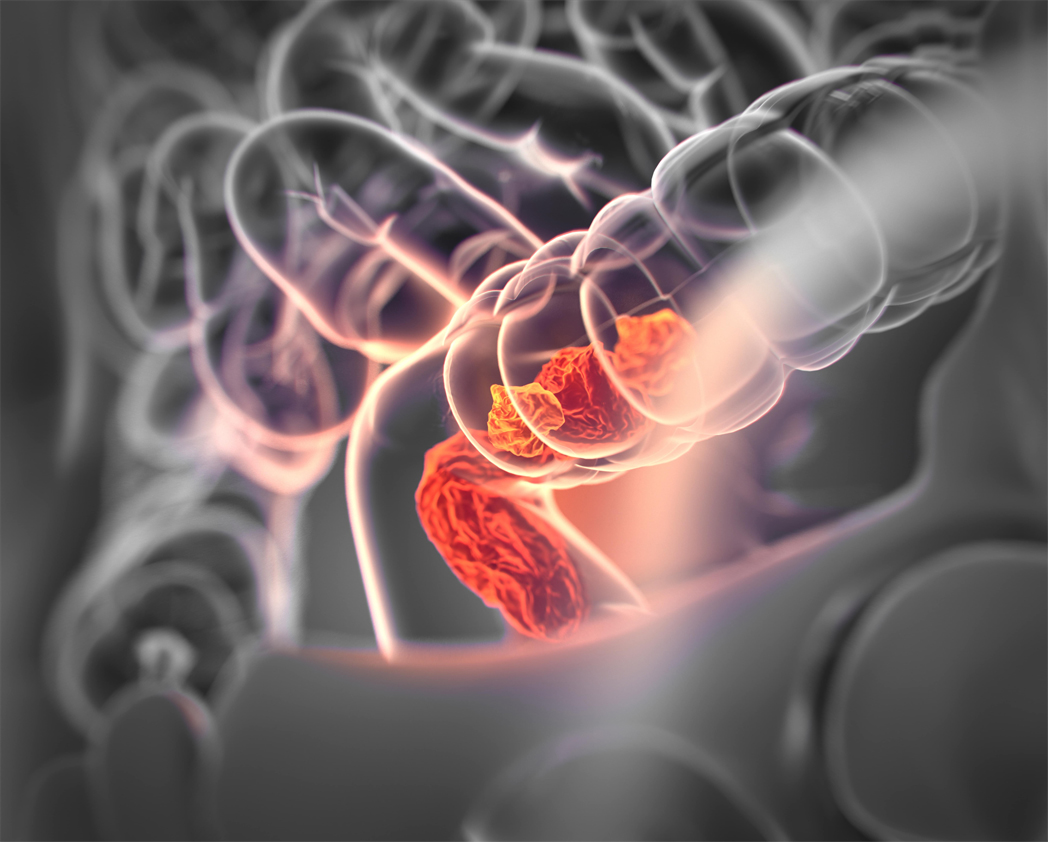
Incident cases of colorectal cancer, the third leading cause of cancer deaths worldwide, more than doubled between 1990 and 2019. For the Global Burden of Disease Study 2019, the Colorectal Cancer Collaborator Network, which includes Khalifa University’s Dr. Juan Acuna, investigated the global impact of colorectal cancer with the results published in the Lancet.
In 2019, colorectal cancer was the third leading cause of cancer deaths worldwide and the second leading cause of disability-adjusted life years (DALYs) for cancer. Around 60 to 75 percent of colorectal cancer cases occur sporadically and are associated with modifiable risk and preventable factors – behaviors and exposures that can raise or lower a person’s risk of cancer – whereas 25 to 40 percent of cases are linked to non-modifiable risk factors, which include genetic factors, a personal history of polyps or adenoma, or a family history of colorectal cancer or hereditary risk.
Incident (new) cases are growing rapidly around the world, but particularly in low-income and middle-income countries. Part of this is due to the increased prevalence of modifiable risk factors, such as smoking, alcohol consumption, unhealthy diets, sedentary behavior, and obesity. However, at the same time, and in contrast, it is now much more affordable and simple to screen for colorectal cancer, with capacity for screening and increasing awareness contributing to the detection of more and earlier cases simply due to more people being screened and to massive programs aiming at early detection. Early detection dramatically improves the prognosis of colon cancer.
Target 3.4 of the UN Sustainable Development Goals focuses on reducing premature mortality from non-communicable diseases, including cancers, by a third by 2030. We can reach that goal by primary prevention (preventing the disease to happen in the first time) or by early detection, when the prognosis is substantially better, including allowing for complete cure. Colorectal cancer is one of those cancers that can be prevented (modifying behaviors or exposures) or detected early. By improving lifestyle and championing early detection we can address the global colorectal cancer burden, making it a key driver of progress towards meeting this goal.
To identify where progress is being made and where more work is needed, recent changes in the colorectal cancer burden should be tracked at the global, regional, and national levels. This global study with the Global Burden of Disease Collaborator Network (more than 700 investigators worldwide) investigated the burden of colorectal cancer in 204 countries and territories from 1990 to 2019. This work built on the previous study conducted in 2017, with another nine countries providing data, adding to the global picture.
In this study the GBD collaborators found that incident cases of colorectal cancer doubled or more than doubled in 16 of 21 world regions, and the number of deaths doubled or more than doubled in 15 of 21 world regions in the past three decades.
When standardized for age, the incidence and death rates either remained the same or decreased in countries measured as high sociodemographic index (SDI) countries, but increased in low SDI and middle SDI locations. Large increases in colorectal cancer incidence rates were observed in middle SDI countries, as well as in people aged 20 to 49 in high SDI countries.
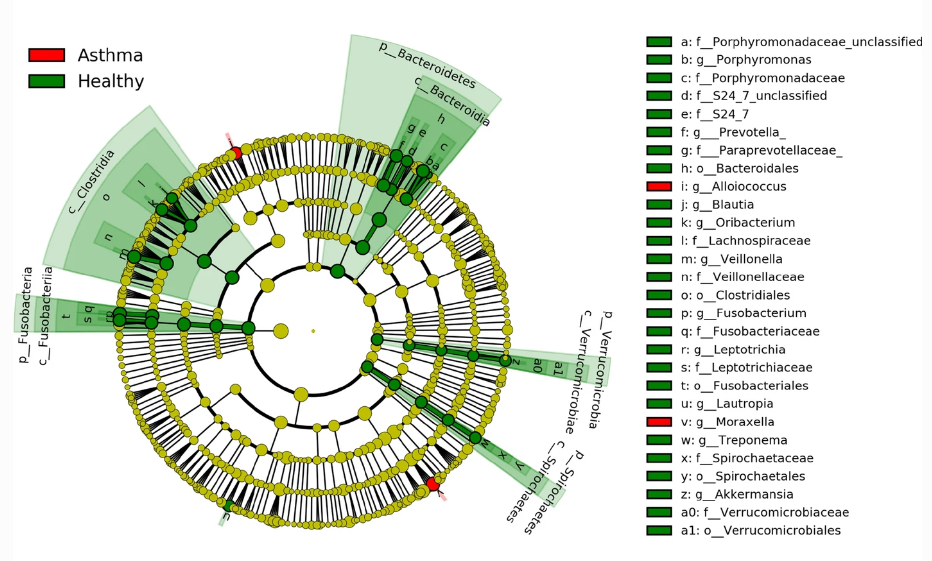
We need further research into why younger people saw an increase in cases, but we can assume some of this is due to the main risk factors for colorectal cancer: obesity, physical inactivity, alcohol consumption, smoking, and an altered gut microbiome. This is where public health interventions can help, including increased screening and awareness and encouraging a reduction in risky behavior.
We can also assume that fast economic growth and rapid industrialization have an impact. A thriving middle class in developing countries adopting a westernized lifestyle characterized by an unhealthy diet and sedentary behavior have resulted in an increased incidence of lifestyle-related illnesses, including colorectal cancer, in the middle SDI countries.
All genders saw an increase in colorectal cancer incidence, but men experienced greater increases in incidence, deaths and disability-adjusted life years (DALYs) than women in terms of absolute counts. In 2019, men accounted for 57.2 percent of colorectal cancer incident cases, and 54.9 percent of deaths due to colorectal cancer. Additionally, when age was taken into account, the preponderance of colorectal cancer in men was more apparent in developed regions, including central Europe, high-income Asia Pacific and Australasia, but differences in the genders were smaller in South Asia and regions of Africa.
China, the USA, and Japan had the highest incident counts for all genders combined, but globally, the age-specific rates of colorectal cancer followed a bell-shaped distribution, with a peak in individuals aged 60 to 74. Incident cases were higher in men than in women in all age groups up to age 80 to 84, with a greater number of new cases in women aged over 85. Incident rates continued to increase with age, but all age groups experienced a rise in incident cases.
At the global level, a diet low in milk (15.6 percent), smoking (13.3 percent), a diet low in calcium (12.9 percent), and alcohol use (9.9 percent) were the main contributor to colorectal cancer DALYs, with the relevant contribution of different risk factors varying as per the region’s development status. A high BMI contributed only 8.3 percent of DALYs, but men with a higher BMI contributed significantly more to DALYs than women.
Colorectal cancer is clearly a global health concern and stemming the tide would be a key contributor to improving health and life quality around the world. We expect low and middle SDI countries to continue to see an increase in cases as a result of population ageing, increased life expectancy and improved screening and detection, so strategies such as dietary and lifestyle modifications are imperative to facing the challenge.
Studies like this one highlight the importance of population-based cancer registries for monitoring colorectal cancer incidence and providing an important resource for people and healthcare providers. Our findings can be used by policy makers and provide new perspectives for scientists and physicians around the world, informing efforts for equitable colorectal cancer control worldwide, with the larger goal of reducing the overall incidence and the specific global burden of cancer for all people.